Cancer Care
Transarterial Chemoembolization (TACE)
What is TACE?
TACE is a minimally invasive procedure used to treat liver tumors and at time other tumors also. It can improve survival rates and quality of life, but it is not a cure.
TACE works in two ways:
- It gives high doses of chemotherapy only to the tumor (to destroy cancer cells)
- It blocks the blood vessels supplying the tumor
Port a Catheter Placement
A port-a-catheter, commonly known as a “port,” is placed under the skin of the upper chest primarily to facilitate cancer treatment. It serves as a long-term access point to a patient’s vein for administering chemotherapy drugs or other medications required during cancer treatment.
Tumor (Cancer) Ablation
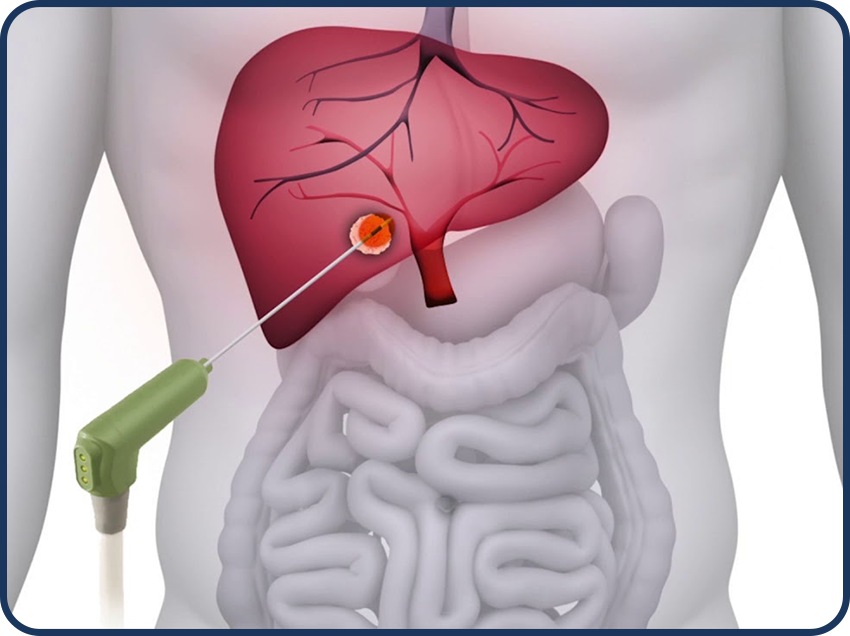
What is Ablation?
Ablation is a procedure that with extreme precision destroys the diseased area of your liver. It uses the energy from electromagnetic waves to heat and destroy the tumor.
At PIIT we manage several tumors using Microware Ablation of the Tumor.
AT PIIT we also manage Cancer patients in a multidisciplinary tumor board. Doctors with specific specialties meet regularly to decide the best treatment plan for each cancer patient. Tumor (Cancer) in the liver can be treated using this minimally invasive technique.
Why Is This Procedure Recommended?
You would be getting this procedure done if you have
- Cancer arising from liver or
- Cancers that have spread to liver from other areas/ organs. (Secondary liver cancer)
How is this procedure performed?
You will be taken into the procedure room and the anesthetist will then give you general
anesthesia.
- Your doctor will prepare the area where the needle is to be inserted with iodine soap and cover it with sterile drape (sheet).
- An ablation needle is placed into the liver tumor through the skin using image guidance (ultrasound or CT scan).
- The ablation needle produces heat which travels a few centimeters, and destroys the tumor and approximately 1-centimeter margin of liver surrounding the tumor.
- At the end of the procedure, the needle will be removed and pressure will be applied to stop any bleeding.
Liver Cancer Treatment Options
At PIIT liver Cancer can be treated with multiple Minimally invasive procedure options. Our Multidisciplinary tumor boards will provide you with the best coarse of treatment. Following are some of the treatment options.
Transarterial Chemoembolization(TACE)
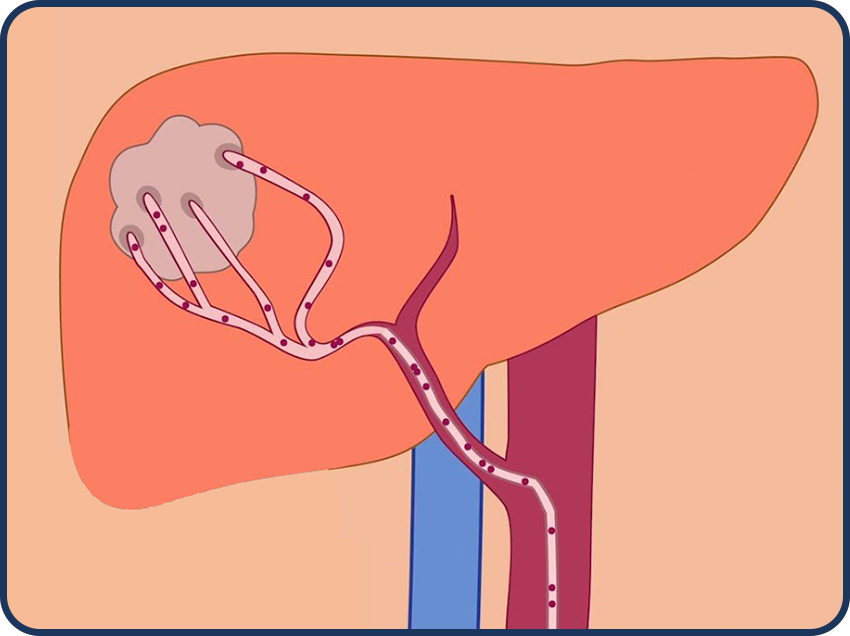
What is TACE?
TACE is a minimally invasive procedure used to treat liver tumors and at time other tumors also. It can improve survival rates and quality of life, but it is not a cure.
TACE works in two ways:
- It gives high doses of chemotherapy only to the tumor (to destroy cancer cells)
- It blocks the blood vessels supplying the tumor
Why Is This Procedure Recommended?
You would be getting this procedure done if you have:
- Cancer arising in the liver or
- Metstatic cancer, which has spread to the liver from somewhere else in the body
How Is This Procedure Performed?
- The procedure begins with the doctor prepping your wrist or upper thigh with antiseptic solution. Some local anesthetic will be injected. This may sting briefly before going numb.
- The doctor will then use another needle to access a blood vessel running up your thigh or a blood vessel going up your arm.
- Once the needle is inside the artery, wire and catheter are used to travel up to the arteries supplying the liver.
- X-ray images or pictures are taken by a special X-ray machine after injecting X-ray contrast sometimes referred to as ‘dye’. This is know as angiography.
What Are The Benefits VS Risks?
We have listed down a few benefits and risks below for better understanding
Benefits
- It is a minimally invasive procedure.
- There is no incision.
- Reduces size and growth of the tumor. This benefit lasts for up to 10 to 14 months depending on the type of tumor. The procedure can be repeated for tumors, that start to grow again.
- Relief of symptoms that are caused by the tumor
Risks
- Bruising at the site of the procedure, which will
eventually resolve. - Pain, nausea and flu-like symptoms may occur.
- Significant bleeding or blockage of artery (rare).
- Infection at area of the liver treated (rare).
- Acute liver failure (rare)
Trans-arterial Radioembolizaion (TARE)-Y-90
What is Radioembolization?
Radioembolization is a minimally invasive procedure used to treat liver cancer. It includes radiation therapy (cancer treatment in which high doses of radiation are used to kill cancer cells) and embolization (blocking blood vessels to prevent blood flow).
It’s a targeted liver tumor therapy that delivers millions of tiny radioactive beads known as Y-90 microspheres (small particles injected into blood vessels to kill tumors) straight to the tumors.
The first ever treatment with this procedure in Pakistan was performed at Doctors Hospital and Medical Center, Lahore.
Why Is This Procedure Recommended?
You will be getting this procedure done if you have Cancer arising from liver (hepatocellular carcinoma, cholangiocarcinoma), or Cancers that have spread to the liver from other areas/ organs. (Secondary liver cancer)
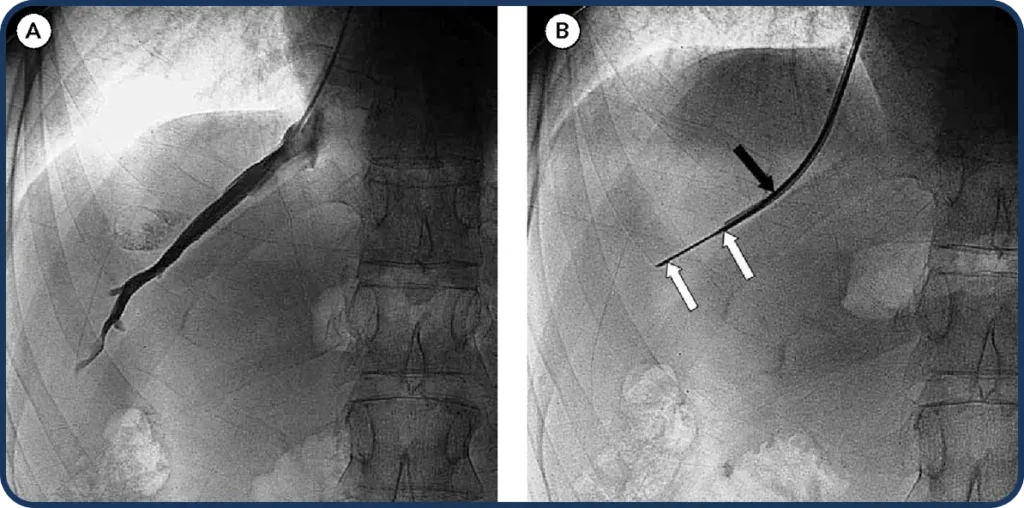
How is this procedure performed?
Step 1:
- TARE Planning which may take 2 to 4 hours to perform begins with the doctor prepping your groin or wrist area with iodine soap.
Local anesthesia will be injected into the skin at the insertion site. You may feel some stinging at the site for a few seconds once the local anesthetic is injected. - After the area is numb, a tube (catheter) is inserted into the blood vessel and navigated to the liver blood vessels. A dye is injected to differentiate the vessels supplying the tumor from the vessels supplying normal liver tissue and other organs. The doctor may block some vessels to minimize the potential for the microspheres to travel to areas outside your liver.
- Next, you will receive a CT scan with dye injected through the catheter to measure the volume of tumor and normal liver. Finally, you will return to the angiography department for injection of a regular radiotracer (Technetium 99m MAAJ to simulate how the radiation spreads in your liver.
- Then, you will be taken to the nuclear medicine department for another scan that measures how the radiation has spread The TARE planning procedure uses a simple form of radiation that does not damage any cells to simulate what will happen when the yttrium-90 will be injected. It also helps in calculating the best dose of radiation to kill the tumor.
Step 2:
- The TARE treatment prepping will begin the same way as the TARE planning procedure.
Once again, a small tube (catheter) is advanced through your wrist or groin and advanced to branches of the hepatic (the artery that supplies the liver) artery to a pre-determined position based on the planning arteriogram. - Once the micro catheter is in the correct position, millions of microspheres (tiny particles injected into blood vessels to kill tumors) with Yttrium-90 are injected through the catheter to the tumor. Radiation from these microspheres will only target the tumor over the next 10 days, but would continue to work for several weeks The catheter is removed once the procedure is complete
What Are The Benefits VS Risks?
We have listed down a few benefits and risks below for better understanding
Benefits
- Kill the tumor.
- Reduce the size of a tumor so that surgery can be performed.
- Slow the development of cancer cells or kill cancer cells and give a patient more time to receive a transplanted organ
- Help reduce symptoms.
- Improves quality of life
Risks
- Infection
- Bleeding or bruising
- Injury to a blood vessel
- Leukopenia (a reduction in disease-fighting cells)
- Radiation pneumonitis (radiation damage to the lungs causing a cough or shortness of breath)
- Radiation ulcer (damage to the bowel causing severe heart burn)
- Radiation cholecystitis (damage to the gallbladder, usually relieved with antibiotics)
Transjugular Liver Biopsy
What is Transjugular Liver Biopsy?
A transjugular liver biopsy is a procedure that involves taking a sample of tissue from your liver. The tissue is then examined and analyzed in the laboratory.
Why Is This Procedure Recommended?
A liver biopsy is a procedure used to detect liver disease by assessing liver tissue in a laboratory setting. A liver biopsy is performed to:
- Diagnose liver disorders that aren’t detectable using less invasive methods.
- Take tissue from a liver problem that was diagnosed via imaging testing.
- Diagnose and stage the severity of liver illnesses such as.
- Liver cirrhosis (healthy liver tissue is replaced with scar tissue, and the liver is permanently damaged).
- Liver cancer.
- Nonalcoholic fatty liver disease (build-up of fat in the liver).
- Hepatitis (inflammation of the liver).
- Primary sclerosing cholangitis (Scars form inside the bile ducts as a result of inflammation).
- Genetic liver diseases
How is this procedure performed?
- The procedure begins with the doctor prepping your right-side neck area with iodine soap.
- Local anesthesia will be injected into the skin at the insertion site. You may feel some stinging at the site for a few seconds after the local anesthetic is injected.
- After the area is numb, a contrast dye is injected.
- A thin needle is inserted through the skin under ultrasound guidance into the neck vein.
- A small tube (catheter) is passed through the veins to your liver. Once the catheter is in the liver, a series of x-rays are taken
- A biopsy needle is passed to the liver via the vein, and typically one to three tiny samples of liver tissue are taken.
- When the procedure is complete, the radiologist removes the tube.
What Are The Benefits VS Risks?
We have listed down a few benefits and risks below for better understanding
Benefits
- Minimally invasive procedure.
- It prevents internal bleeding
Risks
- Bleeding
- Infection
- Damage to surrounding structures
- Irregular heartbeat
- Hematoma (collection of blood)
- Puncture of the lung
Hepatic Artery Embolization
What is an Hepatic Artery Embolization?
Hepatic artery embolization is a minimally invasive procedure used to treat liver tumors and at the same time other tumors also.
This procedure simply blocks blood supply by using specialized medical devices. The tumor itself is not treated.
Why is this procedure recommended?
This procedure is recommended in the following conditions:
- Primary liver cancer (cancer arising from the liver)
- Metastatic cancer, which has spread to the liver from somewhere else in the body
- Failure of chemotherapy, either systemic or intra-arterial infusion (within blood vessels)
How is this procedure performed?
- The procedure begins with the doctor prepping your groin area with iodine soap.
- Local anesthesia will be injected into the skin at the insertion site. You may feel some stinging at the site for a few seconds after the local anesthetic is injected.
- After the area is numb, a contrast dye is injected.
- Under image guidance, a catheter is threaded through a guidewire into the hepatic artery that supplies blood to the liver.
- A series of x-rays are taken to make sure the catheter is in right place.
- Once your tumor is located, particles are injected to block the artery
What are the Benefits VS Risks?
We have listed down a few benefits and risks below for better understanding
Benefits
- Help stop the growth of tumors in your liver or even shrink the tumors.
- It can be used with other treatments like chemotherapy.
- It can be done to control blood loss or shrink tumors before surgery.
Risks
- Infection
- Cholecystitis (redness and swelling of the gallbladder).
- Pancreatitis (inflammation in the pancreas).
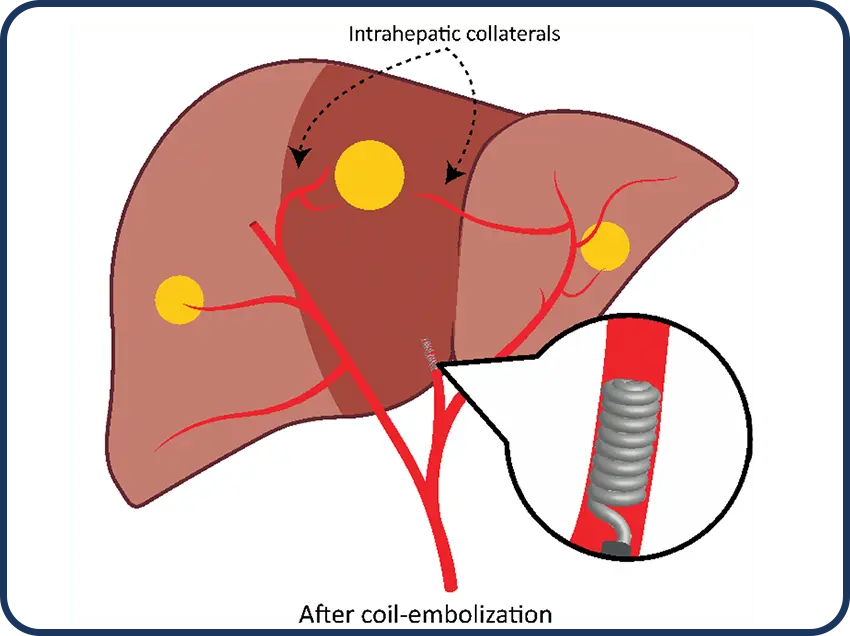
Portal vein Embolization
What is Portal Vein Embolization?
A Portal Vein Embolization (PVE) is a procedure that involves blocking the blood supply to one of the liver lobes (part of liver) while redirecting portal blood flow to the other lobe. The size of the future liver residual (the part of the liver that will be left behind after liver resection) will be enlarged as a consequence of this diversion, which will improve surgical outcomes by preventing liver insufficiency.
Why is this procedure recommended?
This procedure is recommended in a variety of cases which includes:
- A future liver residual (the part of the liver that will be left behind after liver resection) that would be too tiny concerning the patient’s body weight
- Primary liver cancer (cancer arising from the liver)
- Colorectal liver metastasis (tumor from colon spreads to the liver)
- Patients who undergo hepatotoxic (damaging to liver cells) chemotherapy
- Cirrhosis (Healthy liver tissue is replaced with scar tissue and the liver is permanently damaged)
- Hepatic steatosis (fat builds up in the liver)
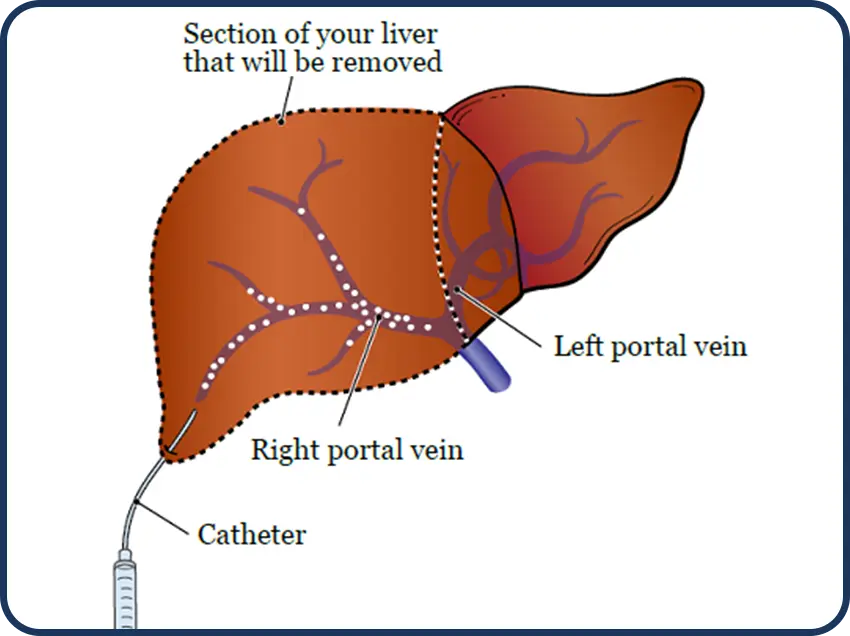
How is this procedure performed?
- The procedure begins with the doctor prepping the area just below your ribcage with iodine soap
- Local anesthesia will be injected into the skin at the insertion site. You may feel some stinging at the site for a few seconds after the local anesthetic is injected
- After the area is numb, a contrast dye is injected
- A tube is inserted into a portal vein through your liver and then a series of wires and catheters are inserted to reach the portal vein.
- Special medical glue is injected into the necessary branches of the portal vein to block them.
What are the Benefits VS Risks?
We have listed down a few benefits and risks below for better understanding
Benefits
- Minimally invasive procedure
- Encourages enough liver to regenerate to allow for resection of cancerous liver
Risks
- Infection
- Bleeding or bile leakage from liver
- Insufficient liver growth
- Leakage of adhesive into other parts of the circulation
Thyroid Biopsy
The thyroid gland, situated in the front of your neck, can develop various nodules/masses for different reasons. When imaging and lab tests aren’t conclusive, your clinician may suggest a thyroid biopsy.
During a thyroid biopsy, the clinician extracts tiny pieces of the nodules/masses for microscopic examination to establish a diagnosis. While many nodules/masses turn out to be harmless, some may indicate more serious conditions like cancer. The biopsy results help your clinician determine the appropriate treatment plan.
You’ll lie on your back as the clinician employs ultrasound to locate the nodules/masses. After numbing the skin, they’ll insert a very thin needle into the thyroid nodules/masses to obtain several samples. They may also use a needle that emits clicking sounds while collecting samples. Following the biopsy, the clinician will cover the pinhole in your skin with a bandage.
How is a Thyroid Biopsy Performed?
You’ll lie on your back as the clinician employs ultrasound to locate the nodules/masses. After numbing the skin, they’ll insert a very thin needle into the thyroid nodules/masses to obtain several samples. They may also use a needle that emits clicking sounds while collecting samples. Following the biopsy, the clinician will cover the pinhole in your skin with a bandage.

