Gastrointestinal Condition
Feeding Tube (Gastrostomy & Jejunostomy Tube Placement): For patient who cannot eat
Why Is This Procedure Recommended?
A feeding tube is a method used to provide food, liquids, and medications to individuals who are unable to consume them orally. These tubes are inserted through the skin and into the stomach.
There are various types of feeding tubes available. The most common type is the gastrostomy tube (G-tube), which terminates in the stomach. Individuals with severe reflux or those whose stomachs do not empty properly may require a specialized feeding tube known as a gastrojejunostomy tube (GJ-tube). A GJ-tube enters the stomach but terminates in the bowel. Another type is the jejunostomy tube (J-tube), which directly enters the bowel.
The insertion of a feeding tube into the body can be performed through surgery, with the assistance of an endoscope passed down the throat, or at PIIT we offer a minimally invasive placement using X-Ray image guidance.
How Is This Procedure Performed?
During the procedure, you will lie on your back and receive medication to induce relaxation. The clinician will inflate your stomach using a thin tube passed through your nose into your stomach, and you’ll be asked not to expel the air. They will then numb your skin and insert the feeding tube through a hole in your abdomen, guided by moving X-rays. The tip of the tube may have a balloon or coil to prevent it from slipping out. Additionally, small buttons may be placed to secure the stomach close to the skin, with instructions provided on their removal if necessary.
Biliary Drainage, Ballooning & Stenting
Why Is This Procedure Recommended?
The liver produces bile, a dense yellow-green fluid crucial for digesting fat in food. Bile flows through specialized channels called bile ducts, with the gallbladder serving as its storage reservoir.
However, bile ducts are susceptible to blockages caused by various factors such as gallstones, infections, inflammation, or cancer. When blockages occur, bile can accumulate and lead to illness. Symptoms may include itching, yellowing of the eyes and skin, pain in the upper right abdomen, and potentially life-threatening infections.
How Is This Procedure Performed?
The procedure begins with the doctor prepping the upper part of the abdomen with iodine soap.
- You will have an injection of local anesthetic in the skin at the site for the thin needle The local anesthetic may sting for a brief period.
- After the area is numb, a needle is put into the liver. Contrast medium is injected into the liver and bile ducts. This helps the duct system show up clearly on X-rays.
- A thin, flexible tube (catheter) is put in and moved into the liver. The doctor uses X-ray or ultrasound pictures as a guide. They then move the catheter into the duct that needs to be drained.
Bile drains through the catheter out of your body. A bag is attached to the end of the catheter to
collect the bile as it drains.
- If a permanent stent is being put, it will be done through the same point, but you will probably have a small tube on the outside for few days.
- Occasionally a sample of tissue is needed to diagnose the cause of the bile duct narrowing and plan your treatment. This may be obtained by passing a small biopsy needle through a tube (sheath) placed from the site where the needle passes through the skin to the narrowing or blockage of the bile duct.
- Biliary dilatation is when the stricture (narrowing) within the bile ducts is opened with a balloon attached on the end of a catheter. This balloon is inflated at the point of narrowing to stretch the duct open.
TIPS & Portal Hypertension Management
What is Transjugular Intrahepatic Portosystemic Shunt?
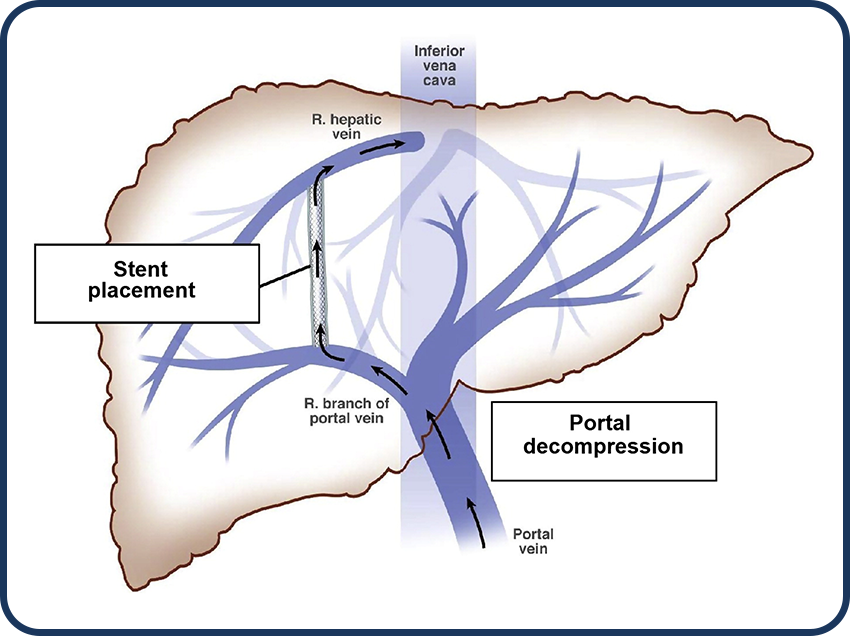
A Transjugular Intrahepatic Portosystemic Shunt (TIPS) is a tract created within the liver to connect two veins within the liver.
Why Is This Procedure Recommended?
- The procedure begins with the doctor prepping the area just above your right collarbone with iodine soap
- Local anesthesia will be injected into the skin at the insertion site. You may feel some stinging at the site for a few seconds after the local anesthetic is injected.
- After the area is numb, a contrast dye is injected into the vein.
- A very small skin incision is made at the site, using ultrasound, the doctor will identify your internal jugular vein, which is situated above your collarbone, and guide a catheter, a long, thin, hollow plastic tube into the vessel.
- Using x-ray guidance, your doctor will then guide the catheter toward the liver and into one of the hepatic veins.
- Access is then gained from the hepatic vein into the portal system using a TIPS needle.
- A stent is then placed under fluoroscopy extending from the portal vein into the hepatic vein.
- Once the stent is in the correct position, the balloon is inflated, expanding the stent into place.
- The balloon is then deflated and removed along with the catheter.
How Is This Procedure Performed?
- The procedure begins with the doctor prepping your wrist or thigh area with antiseptic solution some local anesthetic will be injected. This may sting briefly before going numb.
- The doctor will then use another needle to access a blood vessel running up your thigh or a blood vessel going up your arm.
- The doctor would then insert a small tube(sheath). This will be used as a guide to put the catheter into the blood vessel that is to be blocked.
- X-ray images or pictures are taken by a special X-ray machine after injecting X-ray contrast sometimes referred to as ‘dye. This is known as angiography and helps find the blood vessels that supply blood to the fibroids.
- Fluid containing thousands of tiny particles is then injected through the catheter into these arteries to block them. These particles do not have any side effects and cannot move into other parts of the body.
- The sheath and catheter will be removed after the embolization is done.
- The patient may be required to stay overnight
What Are The Benefits VS Risks?
We have listed down a few benefits and risks below for better understanding
Benefits
- Minimally invasive
- Shorter recovery time
- It replicates the same physiological effects of bypass surgery
Risks
- Infection
- Bruising or bleeding at the insertion site
- Damage to the blood vessel
- Muscle stiffness in the neck
Cholecystostomy tube: Drainage of Bile in Gallbladder
Why Is This Procedure Recommended?
The gallbladder is a small pouch located under your liver that stores a fluid called bile, which is yellow-green in color. When you eat, the gallbladder releases bile into your intestines through a narrow tube. Bile plays a vital role in helping your body digest fat. However, if this tube becomes blocked by a gallstone or sludge, it can lead to an infection in the gallbladder, which can be severe and potentially life-threatening.
In cases where surgery to remove the gallbladder is not feasible, a gallbladder drain, also known as a “cholecystostomy tube,” is an alternative option. This is a thin plastic tube that is inserted to drain pus from the infected gallbladder into a bag.
How Is This Procedure Performed?
The doctor starts by numbing the skin on the right upper belly. They then make an extremely small hole. Through this hole, the doctor carefully inserts a drain into the gallbladder. They use ultrasound and/or real time X-rays images to guide the drain safely into place.
The gallbladder drain needs to remain in position for at least 6 weeks to allow the body to heal around it and prevent bile from leaking out. Bile can be very irritating to the skin and abdomen if it leaks.
Once the blockage is resolved or if the gallbladder is removed during surgery, the gallbladder drain can be taken out. After removal, the hole usually closes on its own within a few days without needing stitches. In rare cases where a patient requires long-term drainage, the drain may need to be replaced with a fresh one every few months.
Percutaneous Transhepatic Biliary Drainage (PTBD)
What is PTBD?
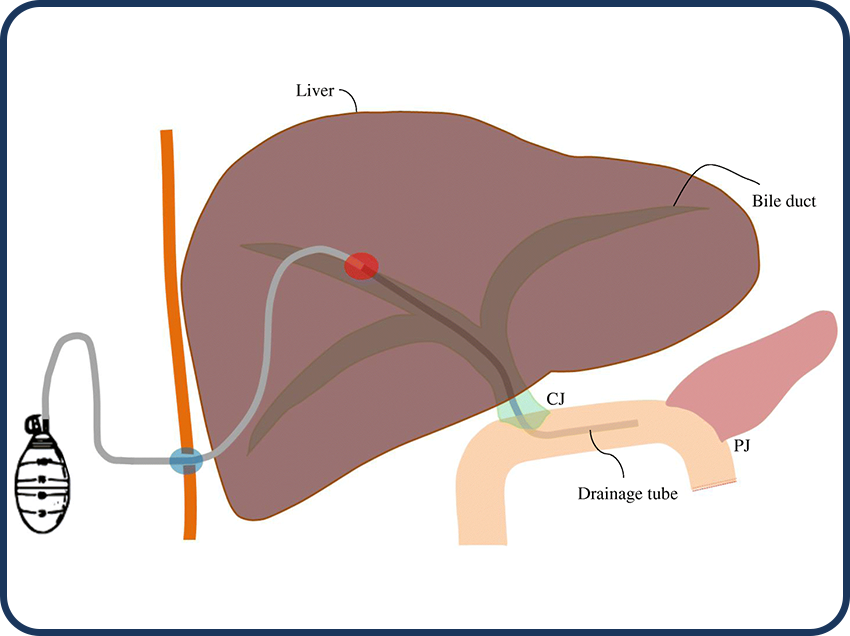
PTBD is a procedure to drain bile to relieve pressure in the bile ducts caused by blockage.
Why Is This Procedure Recommended?
Most common indication for PTDB is blockage or abnormal narrowing (stricture) of the bile ducts.
Conditions that can cause this include:
- Gall stones (stones in the gallbladder or within bile ducts)
- Tumors of the bile ducts, liver, gall bladder or pancreas
- Pancreatitis (inflammation of the pancreas)
- Sclerosing cholangitis (a type of inflammation of the bile ducts)
- Enlarged lymph nodes in the region of the liver and pancreas
- Postoperative strictures (narrowing of the bile ducts or perforation due to injury to the bile ducts during surgery)
- Perforation (a small hole along the bile duct)
- Infection
How Is This Procedure Performed?
- The procedure begins with the doctor prepping the upper part of the abdomen with iodine soap.
- You will have an injection of local anesthetic in the skin at the site for the thin needle The local anesthetic may sting for a brief period.
- After the area is numb, a needle is put into the liver. Contrast medium is injected into the liver and bile ducts. This helps the duct system show up clearly on X-rays.
- A thin, flexible tube (catheter) is put in and moved into the liver. The doctor uses X-ray or ultrasound pictures as a guide. They then move the catheter into the duct that needs to be drained.
- Bile drains through the catheter out of your body. A bag is attached to the end of the catheter to
collect the bile as it drains. - If a permanent ste.nt is being put, it will be done through the same point, but you will probably have a small tube on the outside for few days.
- Occasionally a sample of tissue is needed to diagnose the cause of the bile duct narrowing and plan your treatment. This may be obtained by passing a small biopsy needle through a tube (sheath) placed from the site where the needle passes through the skin to the narrowing or blockage of the bile duct.
- Biliary dilatation is when the stricture (narrowing) within the bile ducts is opened with a balloon attached on the end of a catheter. This balloon is inflated at the point of narrowing to stretch the duct open.
What Are The Benefits VS Risks?
We have listed down a few benefits and risks below for better understanding
Benefits
- Improves liver function
- Long-term survival rate
Risks
- Bile leakage
- Haemobilia (bleeding from or into the biliary tree)
- Cholangitis (inflammation of the bile ducts)
- Infection
- Pancreatitis (inflammation of the pancreas)
- Reaction to the contrast medium
Nephrostomy (Placement, Exchange, Ureteral Stent)
What is Nephrostomy?
A nephrostomy is a procedure in which a tube called a catheter is placed into the kidney. It is used to drain urine from your kidney.
Why Is This Procedure Recommended?
This procedure is recommended in patients who have kidney stones that are blocking the ureter (the tube that carries urine from the kidney to the bladder) or bladder (a muscular sac in the pelvis that stores urine).
Individuals that may require nephrostomy may include those who have:
- Damage to the bladder or ureter
- Blockage in the ureter
- Urethral stricture (a narrowing of the ureter that obstructs the flow of urine)
- Tumors causing blockage
How is this procedure performed?
- The procedure begins with the doctor prepping your lower back area with iodine soap
- Local anesthesia will be injected into the skin at the insertion site. You may feel some stinging at the site for a few seconds after the local anesthetic is injected
- After the area is numb, a contrast dye is injected
- Under image guidance, a needle is inserted into your kidney. A guidewire is then passed through a needle and a plastic catheter is placed over the guidewire.
- The catheter is then secured with a suture and a drainage bag is attached
- A stent is placed across the blockage extending from the kidney into the bladder. It is placed through the catheter
- If you require the nephrostomy for a longer time, the nephrostomy tube will need to be exchanged periodically
What Are The Benefits VS Risks?
We have listed down a few benefits and risks below for better understanding
Benefits
- Faster recovery
- Maintain kidney function and protect the kidney from damage and infection
- Help to diagnose an underlying problem
Risks
- Bleeding
- Blood clots
- Infection
- Damage to adjacent organs
- Loss of kidney function

